About our Lymphoedema Service
The Lymphoedema Service in St Margaret’s Hospice accept referrals from any Health Care Professional and will accept patients from Somerset (excluding North Somerset), and out of area referrals for children residing in adjoining counties (primarily North Somerset and North Devon).
Our main clinics are outpatient based within the Taunton and Yeovil Hospice sites; however, we also provide outreach clinics in several community hospitals across the county for our stable clients.
We can also offer video call consultations with patients, carers, and other health care professionals.
The Lymphoedema Service is provided by experienced Health Care Professionals with specialist qualifications in Lymphoedema Management from one of the four International Schools of Lymphoedema Training (Foeldi, Leduc, Casley-Smith and Vodder). The service provides a skill mix of staff comprising of Lymphoedema Specialists, Lymphoedema Keyworkers, Lymphoedema Assistant Practitioners, Lymphoedema Health Care Assistants, Lymphoedema Administrators, and volunteers.
What our Lymphoedema Service does
Although lymphoedema cannot be cured, it can be managed well by a combination of elements. Our lymphoedema team provides education and support, helping to ease client’s discomfort and teaching them how best to manage their symptoms:
Such as: –

- Teaching to look after skin correctly and why this is important
- Promoting exercise and weight management
- Providing compression therapy
- Teaching patients simple lymphatic drainage massage
- Prophylactic monitoring service
- Kinesio taping
- Laser light therapy
- Intensive bandaging treatments
- Manual lymphatic drainage/hivamat.
We encouraged our clients to participate in supporting their treatment plan, working towards self-management.
What to expect at your first appointment
 Your initial appointment could be between one and two hours and you will be seen by one of the Lymphoedema Clinicians, who will assess you and aim to give a diagnosis. During your appointment you will be asked to remove any necessary garments, so that we can examine both the swollen and adjoining areas.
Your initial appointment could be between one and two hours and you will be seen by one of the Lymphoedema Clinicians, who will assess you and aim to give a diagnosis. During your appointment you will be asked to remove any necessary garments, so that we can examine both the swollen and adjoining areas.
You may be asked to transfer onto a couch to enable us to assess you. If you have difficulty getting in and out of a chair or bed, or need special equipment to help you, please let the clinic know before you come to your appointment.
If you think you would like someone else to be present, you are welcome to bring a friend, family member or carer or ask us to provide a chaperone for you.
At the end of your initial assessment, we will agree a treatment plan tailored to your needs.
What is Lymphoedema?
Lymphoedema is a chronic (long term) condition that causes swelling to appear. It can affect any part of the body but most commonly develops in the arms or legs.
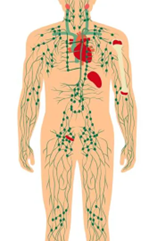
The role of the lymphatic system is to move fluid around our bodies, remove waste products and support our immune system.
This function is gained via a network of vessels, nodes and organs that work alongside the veins/venous system to remove all fluids that leak out of blood vessels. This fluid is called lymph and is passed around the body with a push from lymphatics, a squeeze of the muscles and with the help of gravity to pass it as waste into urine.
Lymphoedema most commonly develops due to the lymphatic system being damaged, blocked, or overloaded. This is known as secondary lymphoedema , because it is secondary to events such as trauma to the lymphatics/veins, surgery to the lymphatics/veins, removal of lymph nodes, obstruction due to cancer cells and overloading of the system due to conditions such as cardiac failure. A reduction of movement or sudden weight gain and obesity can also cause secondary lymphoedema. The body needs to move often to drain and excess fatty tissue restricts drainage.
Finally, a parasite can also enter the body and reside in the lymphatics, again restricting drainage. This is known as filariasis which is more common in tropical countries.
Primary lymphoedema is less common but is caused by alterations (mutations) in genes that are responsible for the development of the foetal lymphatic system in utero. This commonly develops from birth but can manifest at times of hormone change such as puberty, pregnancy, or menopause.
Unfortunately, we are still unable to predict who is most likely to develop lymphoedema, so when you come to the clinic, we will take a detailed history to try and enable the correct cause and treatment to help you manage your lymphoedema.
Lipoedema is a painful bi-lateral (symmetrical) limb swelling, mainly affecting the legs and thighs but sometimes arms too. It is thought to occur because of an abnormal accumulation of fat cells (unrelated to diet) in the tissues under the skin.
Patients generally present with very large lower limbs that are similar in shape and size on both sides. The thighs, hips and buttocks often tend to be disproportionate (much larger) than the rest of the upper body – the waist is much smaller and the feet and hands are hardly ever affected.
The tissues of the limbs tend to be very tender or painful to touch.
At present, we do not understand why lipoedema occurs, however a family history suggests a genetic basis. It seems to affect females exclusively and it is usually first noticed when there is a hormonal change, such as at puberty or pregnancy, or even the menopause.
Despite the name, oedema is not a feature of lipoedema. However, oedema may be present if the patient has other co-morbidities, such as venous or cardiac insufficiency, reduced mobility or general obesity. It can often be mistaken for other conditions, in particular obesity, as well as Lymphoedema .
There currently is no known cure for lipoedema, but the progression can be minimised by implementing treatment as soon as possible. Getting a diagnosis is therefore essential and will enable women to have the best possible information to manage this often distressing condition. Stabilising weight is thought to be very helpful in preventing progression of the disease.
Assessment is vital to ensure a correct diagnosis is given and appropriate, realistic and achievable goals instigated.
Treatment will include:
- Goal setting
- Support garments, such as sport leggings
- Support with psychological issues
- Movement/exercise
- Managing/stabilising weight (no diets)
- Education to self-manage the condition.
Lipoedema
- Painful swelling of the lower limbs/arms, which is bi-lateral and symmetrical (the same on both sides)
- General body shape is usually disproportionate (small torso, narrow waist and larger hips/thighs)
- Feet or hands are usually not affected
- Pitting (firm pressure on the skin leaving obvious indentations) of the skin is absent
- There is often a family history of the condition
- Generally affects females only
- Losing weight will not make a noticeable difference to the affected areas
- Limbs will often bruise easily and through no apparent cause
- There is sometimes a pad of fat just under the knees and hips.
Lymphoedema
- Swelling may be unequal on each side of body – one limb is often much larger than the other
- Feet are frequently affected and there will be a positive Stemmers sign (inability to pick up a fold of skin at the base of a digit)
- Pitting of the skin will be present – especially in the early stages of the condition
- No pain is felt if pressure is applied to the skin, but there is often a feeling of tightness in the tissues
- Limbs do not tend to bruise easily
- Increased risk of infection (cellulitis) in affected, swollen areas
- Can affect females and males of any age
- The affected skin is often thickened and may have other features such as warty change or papillomatosis (cobble stone effect on the skin)
- Losing weight usually has a beneficial effect on the swelling.

Lymphoedema Resources
Meet the team

Debbie
Lead Lymphoedema Specialist

Debbie
Prior to moving to Somerset in 2013, I led a Lymphoedema Service in Nottingham for 6 years and had the privilege to assess, manage and treat complex patients alongside Professor Vaughan Keeley and Christine Moffatt.
I started leading the Lymphoedema Service here at St Margaret’s in March 2022. I really enjoy working within Lymphoedema and as there continues to be more research and innovation into this specialist area, it is exciting to be part of this development.
My interests
I love the outdoors! I really enjoy keeping active; walking, jogging, cycling and gym classes. I enjoy meeting up with friends and family, going on holiday, cooking, eating out, listening to music, reading…the list goes on!!!
My favourite thing
Family…and chocolate!!

Frances
Deputy Lead Lymphoedema Specialist

Frances
My interests:
I have so many interests and am always busy – the list is endless!!
My favourite thing:
Relaxing with good company and a glass of wine.

Ali
Lymphoedema Specialist

Ali
My interests:
Going moor walking as much as possible, which I combine with going away in my campervan and taking the dogs with me.
My favourite thing:
I love nothing more than spending my time outside or watching a game of tennis with a glass of gin.

Becky
Lymphoedema Specialist

Becky
My interests:
I am kept busy by my three young children and two mad spaniels!
My favourite thing:
Long walks with the dogs.

Aly
Lymphoedema Specialist

Aly
My interests:
Narrow boating, dog, family, swimming, coaching and walking the dog; animals in general, I have plenty of pets.
My favourite thing:
Nature and the outdoors.

Laura
Lymphoedema Specialist

Laura
In 2010 I move my focus into the leg ulcer service, spending days in clinics doing compression bandaging and managing the team. I think after 10 years in this role I could do bandaging with my eyes closed!
In the last few years, I have been a tissue viability nurse specialist (posh way of saying I helped managed wounds and skin care) back in the acute setting.
Throughout all this, my focus has always been on bandaging and how the right care at the right time has the best outcome, so this is the perfect role for me. I still get to bandage, be hands on and give service users the best care I can.
My interests:
I love a good read with a cuppa, or a night out at the cinema. If you want to have a nerdy in-depth chat about DC, I’m your girl.
My favourite thing:
Coffee and chocolate.

Fiona
Lymphoedema Keyworker

Fiona
I started my Health care career in 2008 working as a phlebotomist at a health centre before joining the Somerset Foundation Trust in 2013 and working with the Leg Ulcer Service. During my eight years with the team, I was able to work towards and gain a qualification in adult nursing.
As a qualified nurse I worked across the Bridgwater and Sedgemoor district nursing teams, then with an interest in palliative care worked on the In-Patient Unit at the hospice. I am a firm believer in holistic, patient-lead care which has steered me to the lymphoedema team as it is an integral part of our approach to patient care.
My interests: I love a good podcast on evolutionary psychology and enjoy a good walk and yoga practice. I am a keen gardener and generally love being out in nature, a beer garden will do.
My favourite thing: Sitting down to a family meal and having a good yarn, this traditionally ends in a friendly debate!

